Transforming Payer Operations
The Illuminator helps payers reduce costs, optimize claims, and improve member satisfaction through better caregiver engagement.
Reduce Utilization
Empower caregivers with the information they need to make informed decisions, reducing unnecessary emergency room visits and hospitalizations.
Optimize Policy Claims
Improve claims accuracy and processing efficiency through better documentation and coordination between caregivers and healthcare providers.
Boost Member Satisfaction
Enhance the member experience by providing caregivers with the tools they need to navigate complex healthcare systems effectively.
Key Benefits for Payers
The Illuminator delivers measurable results for healthcare payers
Reduced Healthcare Costs
Studies show that engaged caregivers can help reduce healthcare costs by up to 20% through better care coordination and preventive measures.
Improved Member Retention
Members whose caregivers have access to comprehensive healthcare information are more likely to remain with their current payer.
Enhanced Compliance
Better documentation and care coordination leads to improved compliance with healthcare regulations and quality measures.
Data-Driven Insights
Gain valuable insights into member needs and care patterns to inform policy and program development.
Streamlined Claims Processing
Reduce administrative overhead and processing time with more accurate and complete information from caregivers.
Differentiated Member Experience
Stand out in a competitive market by offering innovative caregiver support tools that improve the overall healthcare experience.
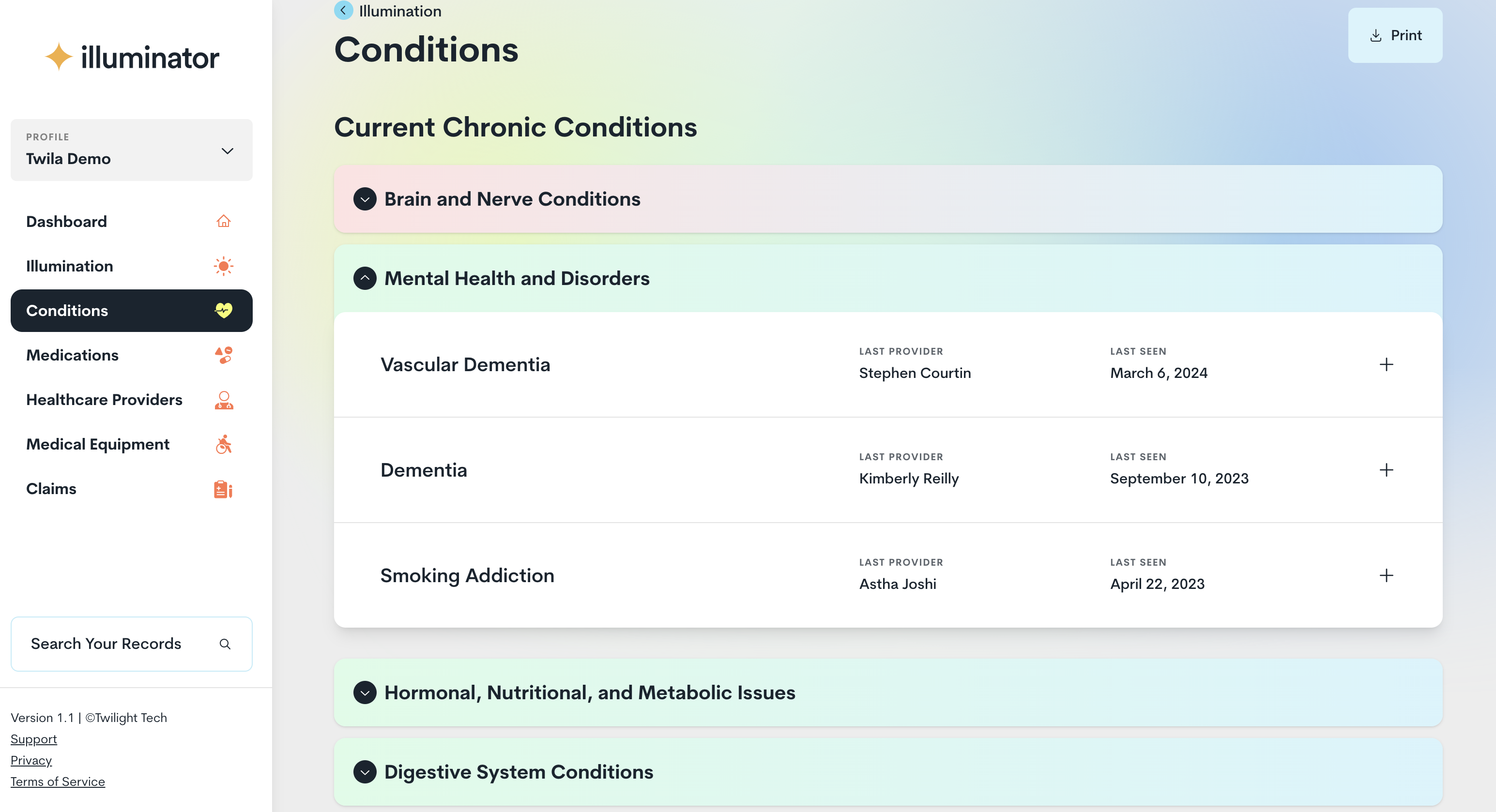
Intelligent Care Coordination
The CareMinders notification system transforms healthcare data into actionable insights, improving chronic disease management and reducing costly interventions.